Blog | 30 Mar 2020
Pandemic hotspots, vulnerable workers: New York, New Jersey & Florida
Three of the most populous states, including hard-hit New York, have aging healthcare workforces that may be more vulnerable to the novel coronavirus pandemic.
The healthcare workforces of New York, New Jersey, and Florida skew older than national averages, including more workers over 60 years old − a key group at risk for coronavirus. New York is the US epicenter for the pandemic, neighboring New Jersey is another early hotspot, and Florida’s caseload is growing rapidly.
A vulnerable healthcare workforce has serious implications for already-stressed health systems. Reports of frontline workers with COVID-19 already have grown frequent − Florida just saw its first fatality, a 67-year-old MD − with an ongoing, nationwide shortage of protective gear making the problem worse.
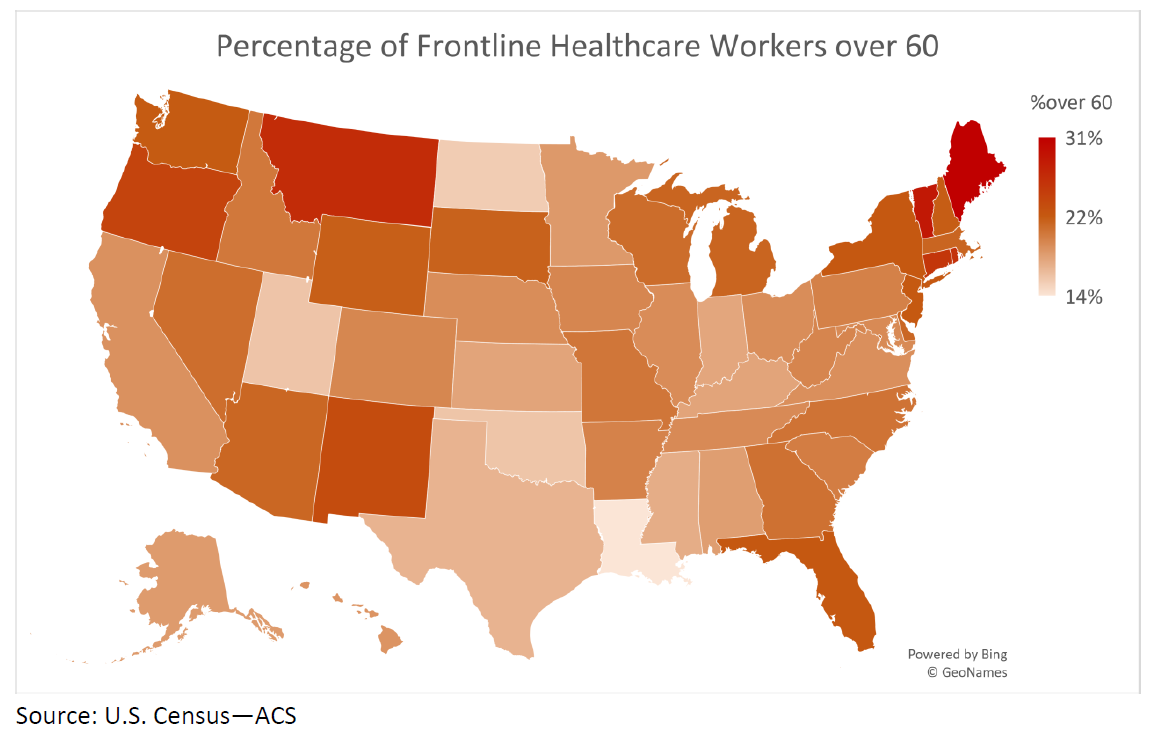
Oxford Economics looked at the demographics of the US healthcare workforce, including frontline occupations (e.g., doctors, nurses, respiratory therapists) facing acute risks of exposure to coronavirus while treating patients in hospitals, nursing homes, clinics, and other facilities. The median percentage of frontline healthcare workers who are older than 60 across the country is 20%, compared to 23% in New York, New Jersey, and Florida. In Maine, nearly one in three frontline workers is over 60; Vermont and Montana also have high percentages of older workers, followed by Connecticut and Oregon.
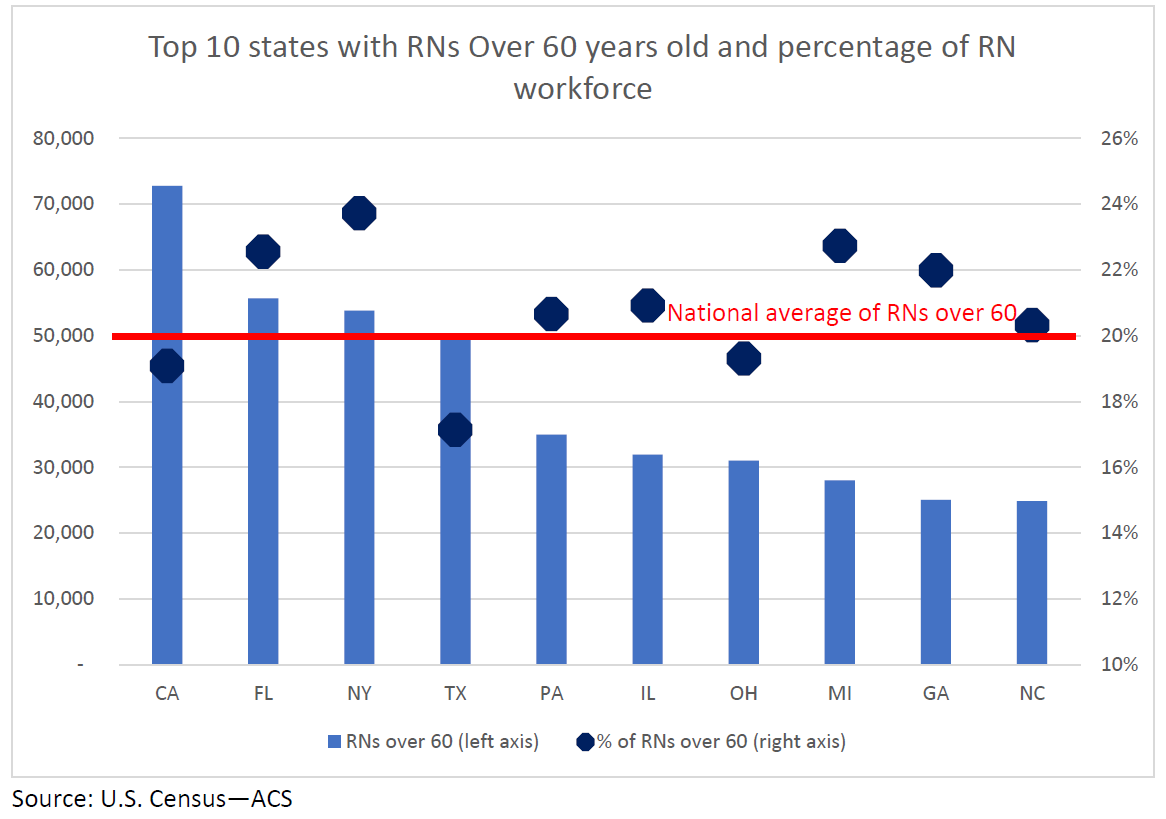
In New York’s critically important nursing sector, including nearly 54,000 registered nurses about one in four are over the age of 60 (the national average of employed RNs over 60 is about one in five). Seven of the 10 most populous states have above-average percentages of RNs over 60.
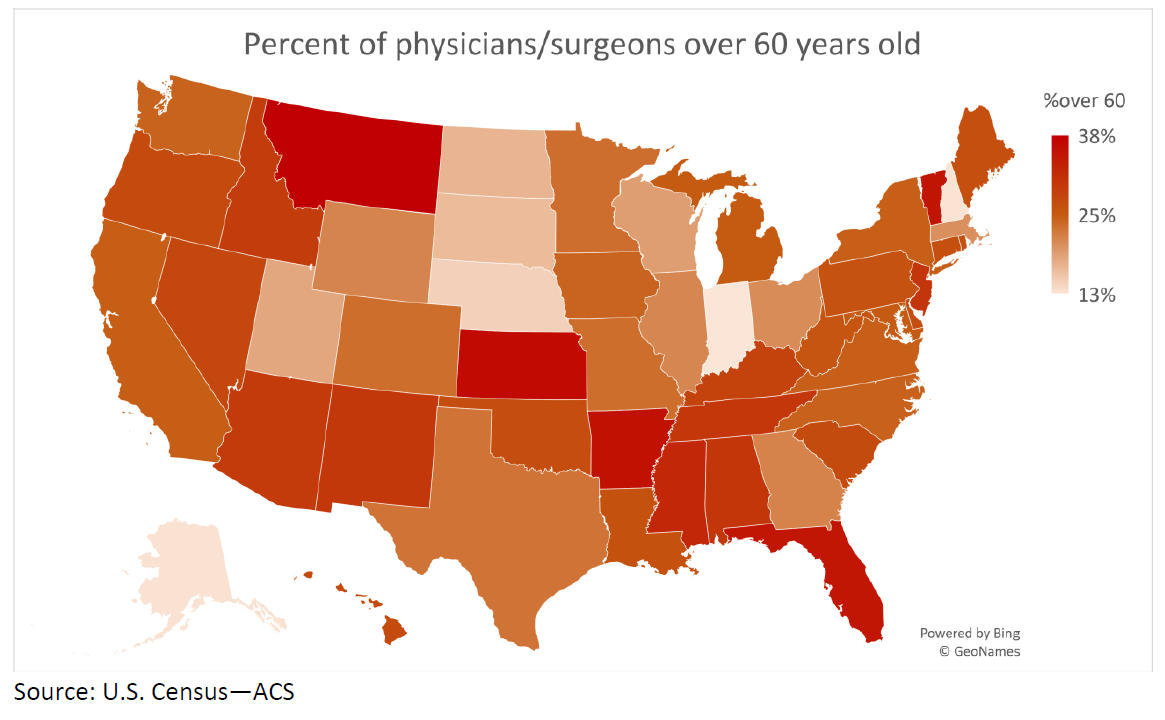
For physicians, the vulnerabilities are even more pronounced. About 25% of medical doctors are over the age of 60. While a handful of states have a larger proportion of younger physicians, many others skew toward much older professionals. In Montana, nearly 40% of MDs are over 60. Highly populous states, including many hard-hit by COVID-19, also tend to tilt toward older physicians. New York matches the national average at 25%, while New Jersey’s is over 30%.
Older workers are an essential part of America’s frontline healthcare workforce. Unfortunately, given the nature of the novel coronavirus, these skilled professionals appear to be at greater risk than their younger peers − at a time when their absence due to illness could make the fight against COVID-19 even more difficult and healthcare systems already face enormous challenges.
Tags:
You may be interested in

Post
Analysing the German construction industry’s supply chains
The supply chain disruptions triggered by the coronavirus pandemic, the blockade of the Suez Canal, and Russia's invasion of Ukraine were historically unique for Germany’s construction sector. Our research showed how these supply chain disruptions affected construction companies in various ways and identified strategies to help overcome them.
Find Out More
Post
Economies with pre-existing conditions suffer bigger Covid scars
We project the distribution of long-term economic pain inflicted by Covid will be similar to humans in the sense that those with pre-existing conditions will end up suffering the most.
Find Out More
Post
Good Practices in the Provision of Global Public Goods: How multilateral development banks build on global public goods in their operations
In our flagship report, ‘Multilateral Development Banks for Global Public Goods’, commissioned by Deutsche Gesellschaft für Internationale Zusammenarbeit on behalf of the German Federal Ministry for Economic Cooperation and Development, Oxford Economics highlighted the positive role that the use of GPGs can play in preventing and addressing crises that cross national boundaries. As part of that work, we wanted to identify and share promising practices and good examples of how the provision of GPGs can be supported through international funding—and in particular through MDBs.
Find Out More